What is Osteoporosis?
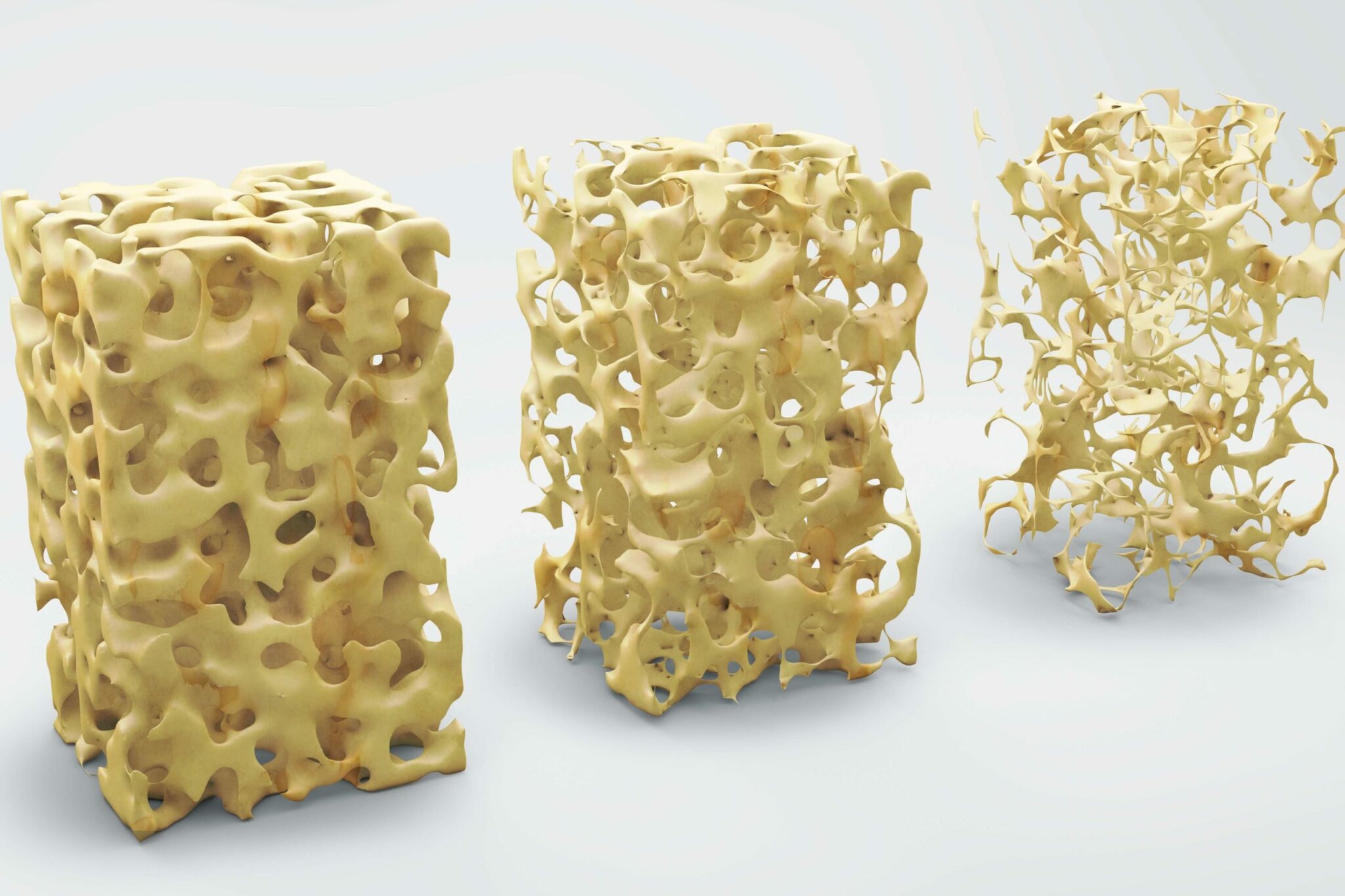
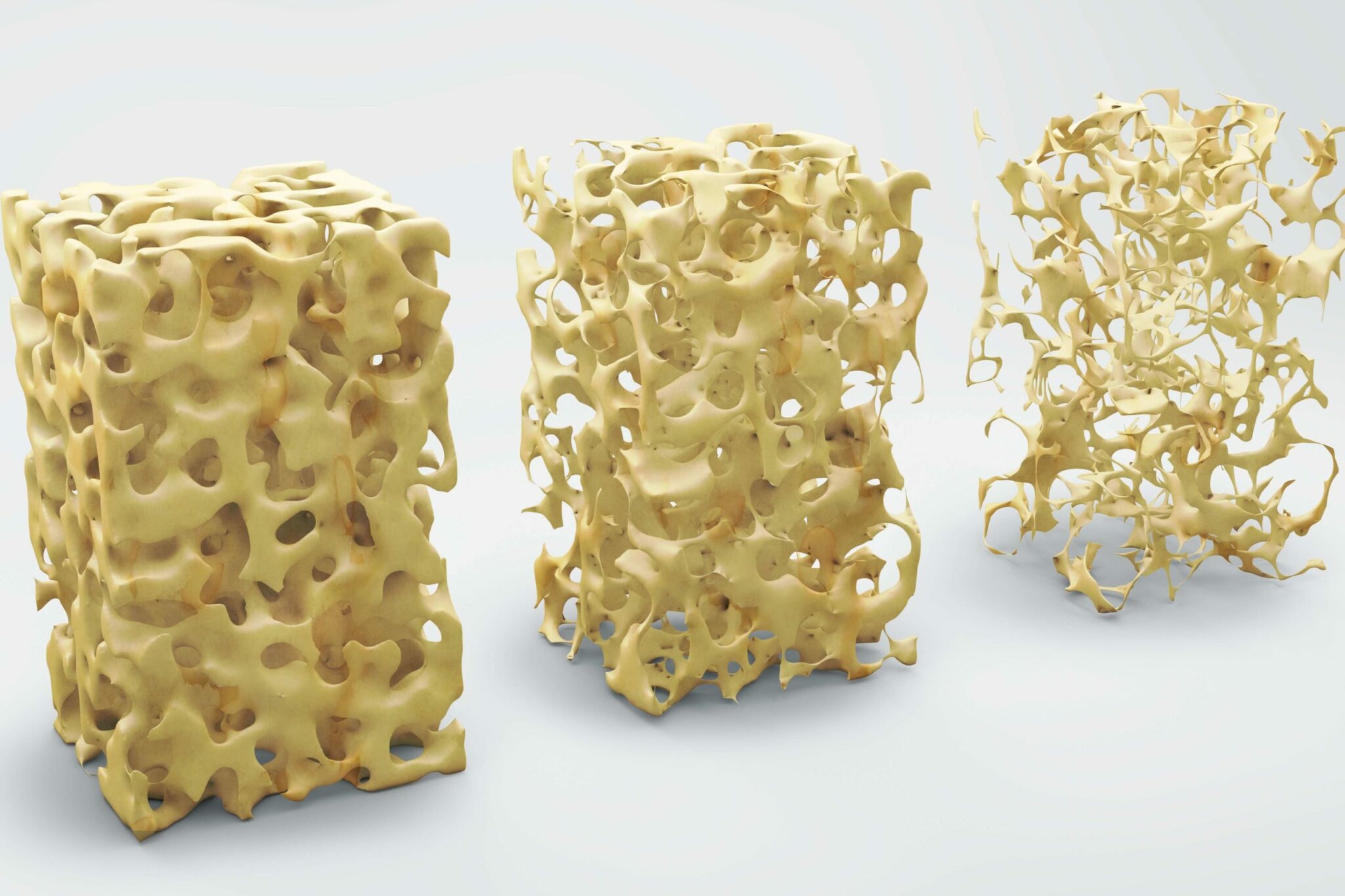
Osteoporosis is a condition that is characterised by brittle bones. The bones become porous and weak, which means that people with the condition are at increased risk of experiencing fractures. Osteoporosis is very common; in fact, it is thought that as many as 50% of women over the age of 50 will suffer an osteoporotic fracture, whilst 24% of men will.
So what causes it? Bone is a dynamic tissue, which means it is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone does not keep up with the loss of old bone. The skeleton becomes less dense as a result and in extreme cases bones can fracture in response to something as innocuous as bending over, or coughing. The most common sites of fracture are the wrist, the hip and the spine.
What are the warning signs for osteoporosis?
Osteoporosis is a challenging condition to prevent because it tends to develop slowly and without warning. Many people only become aware that they have the condition when they experience a fracture, by which time it is too late for preventative measures.
Some people do discover they have osteopenia earlier in life, which is often thought of as a precursor to osteoporosis and happens when bone density is lower than the average for that age. Taking steps to improve your overall bone health following a diagnosis of osteopenia might reduce your risk of developing osteoporosis later in life.
What causes osteoporosis?
Losing bone mass is a normal part of aging. Typically we reach our peak bone mass in our mid 30s and from this point on we continuously lose mass as we age. This loss is accelerated in the first few years after menopause, which is why women of this age are at particularly high risk of osteoporosis. The enhanced loss is thought to be due to declining oestrogen levels.
There are, however, other risk factors, which include:
- Family history.
- Eating disorders and/or a BMI < 19
- Heavy drinking or smoking
- Certain medical conditions, which include:
- Autoimmune (Lupus, arthritis)
- Digestive (celiac disease, inflammatory bowel disease)
- Cancer (breast, prostate)
- Haematologic/blood disorders (multiple myeloma)
- Neurological (multiple sclerosis, stroke)
- Endocrine/hormonal conditions (Cushing’s syndrome, premature menopause, thyroid disorders)
- Medication use. Most notably high dose steroids, used long-term to treat arthritis and asthma. There are also known associations between osteoporosis and some anti-cancer medications (particularly those that are anti-oestrogenic), anti-seizure medications and transplant rejection medicines.
Osteoporosis is less common in men than women, but it does happen. It is not well understood why some men are more susceptible, but there is a link between osteoporosis and reduced testosterone levels.
How is osteoporosis diagnosed?
Osteoporosis is diagnosed using a special low-level X-ray scan, called a dual energy X-ray absorptiometry (DEXA) scan. During this procedure, the density of the bones is measured and compared to the expected bone density of a healthy young adult. Results are expressed as the standard deviation (SD) of the T score:
- T score above -1 SD: Normal
- T score -1 to -2.5 SD: Osteopenia
- T score below -2.5: Osteoporosis
How is osteoporosis managed and treated?
Following a diagnosis of osteopenia or osteoporosis there are lifestyle adjustments you can make to improve your overall health. These include eating healthily and undertaking regular exercise.
Exercise
It is recommended that adults between the ages of 19 and 64 do at least two and a half hours of moderate intensity exercise each week. For optimal bone strength, this should be a combination of weight bearing exercises and resistance training. Weight bearing exercises include walking, aerobic classes and tennis; anything where the legs and feet support the weight of the body. They strengthen the muscles, ligaments and joints. Resistance exercises improve bone strength by encouraging the tendons to pull on the bones. Examples include press-ups and weight lifting. Further medical advice includes reducing the likelihood of falls, so exercises such as Tai-chi that improves balance are worth incorporating into your regular routine.
Diet and supplements
Calcium and vitamin D are very important for good bone health. Calcium is the main mineral found in bone. Most people can get sufficient calcium from their diet, by including foods such as leafy green vegetables, tofu, yoghurt and other dairy products. Women over 50 and men over 70 are recommended to ensure that their daily intake of calcium is between 1000 and 1200 mg. If they struggle to do this through diet alone, calcium supplements should be added to the diet. Vitamin D helps the body to absorb calcium. The main source of vitamin D is the sun, which means that depending on where you live and what time of year it is, you may get sufficient quantities of the vitamin from just spending time outside. In parts of Europe that have limited daylight hours during the winter it can be very difficult to absorb sufficient vitamin D from the sun alone. Likewise, in the Middle East, when temperatures rarely drop below 40°C in the summer months, many inhabitants of the region find that they are deficient in the vitamin. Oily fish, red meat, liver and egg yolks can all help to boost your intake; however, many find that they also require supplements to reach the recommended 10 micrograms a day.
Medications
Whilst medication is not a route that everyone wants to take, the consequences of unmanaged osteoporosis can be severe. As many as 20% of senior citizens who break their hip will die within 12 months, either due to complications or during surgery to repair it. Broken bones in the spine can cause long-term, debilitating pain and a stooped posture; and limited mobility can result in loneliness and depression. There are several drug treatments available for the treatment of osteoporosis:
- Bisphosphonates, such as alendronic acid, ibandronic acid, risedronic acid and zoledronic acid. These can be given intravenously or orally and work by slowing the rate at which old bone is broken down. Side effects include nausea, stomach pains and difficulty swallowing and they can take between 6 to 12 months to exert a positive effect.
- Selective oestrogen receptor modulators (SERMS). The only SERM licensed for the treatment of osteoporosis is raloxifene. SERMs exert a similar effect to the hormone oestrogen, without the associated health risks of HRT (see below). They work by maintaining bone density and reducing the risk of fracture. Side effects include hot flushes, blood clots and leg cramps.
- Parathyroid hormone-like drugs, for example teriparatide. Endogenous parathyroid hormone regulates the amount of calcium in bone. Medications such as teriparatide are given as injections and work to stimulate the production of new bone and therefore, increase bone density. They are usually given in more severe cases of osteoporosis, or when other treatments have failed to work. After two years of treatment, most patients are switched off these drugs and onto medication that will maintain their new bone growth. Nausea and vomiting are common side effects.
- Hormone Replacement Therapy (HRT). HRT is given to many women to relieve the plethora of symptoms they may encounter during their menopausal years. Whilst some women with osteoporosis do take HRT, it is not specifically recommended for treating this condition due to an increased risk of breast cancer, endometrial cancer, ovarian cancer, stroke and venous thromboembolism. If you are considering HRT, it is important to discuss these risks with your doctor prior to commencing treatment.
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
Sources:
- “Learn What Osteoporosis Is and What It’s Caused By.” National Osteoporosis Foundation, 25 Sept. 2020, www.nof.org/patients/what-is-osteoporosis/.
- “Osteoporosis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 19 June 2019, www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968.
- “Osteoporosis.” NHS Choices, NHS, www.nhs.uk/conditions/osteoporosis/.
- “Overview: Raloxifene and Teriparatide for the Secondary Prevention of Osteoporotic Fragility Fractures in Postmenopausal Women: Guidance.” NICE, www.nice.org.uk/guidance/ta161.













































