What are Uterine Polyps?
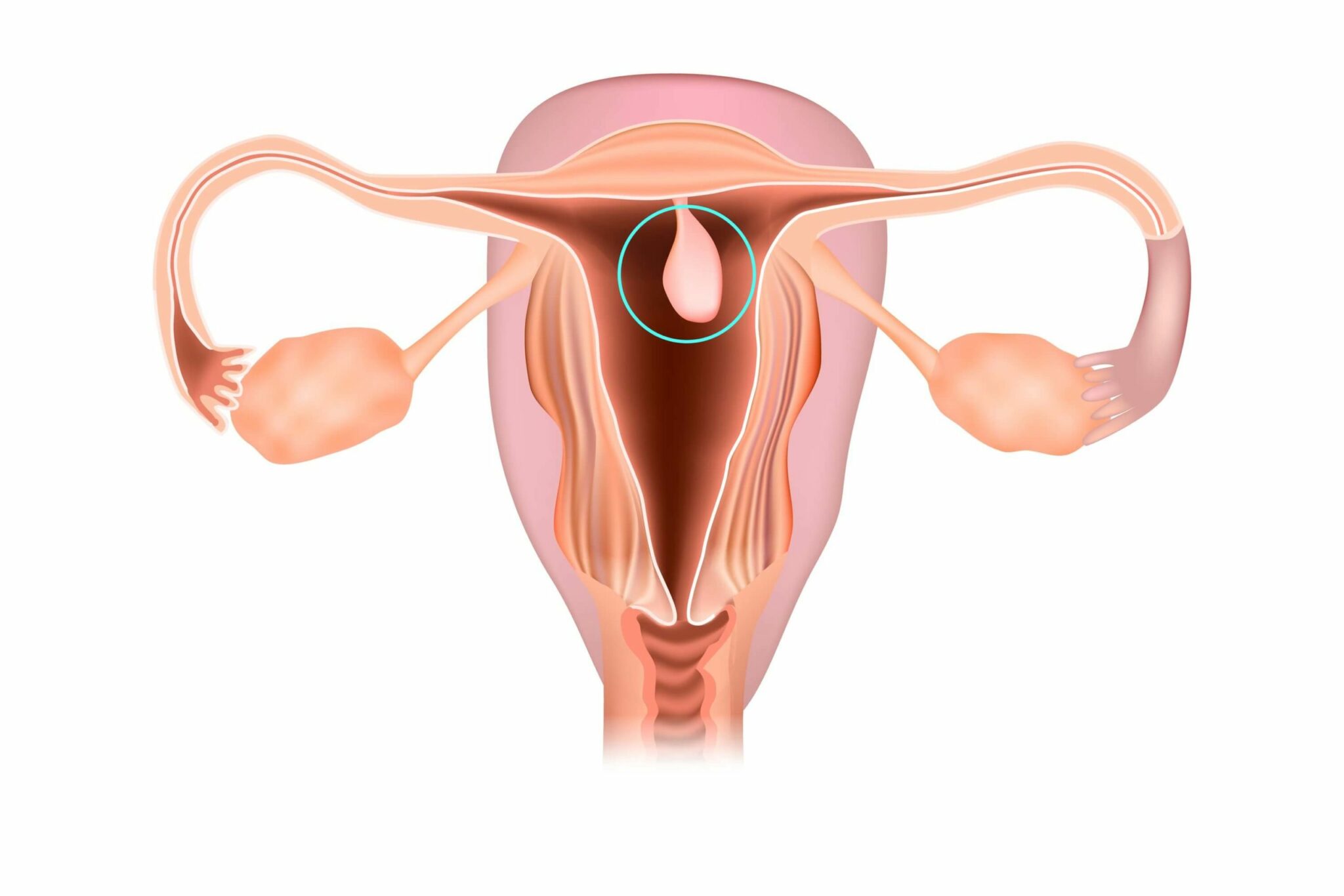
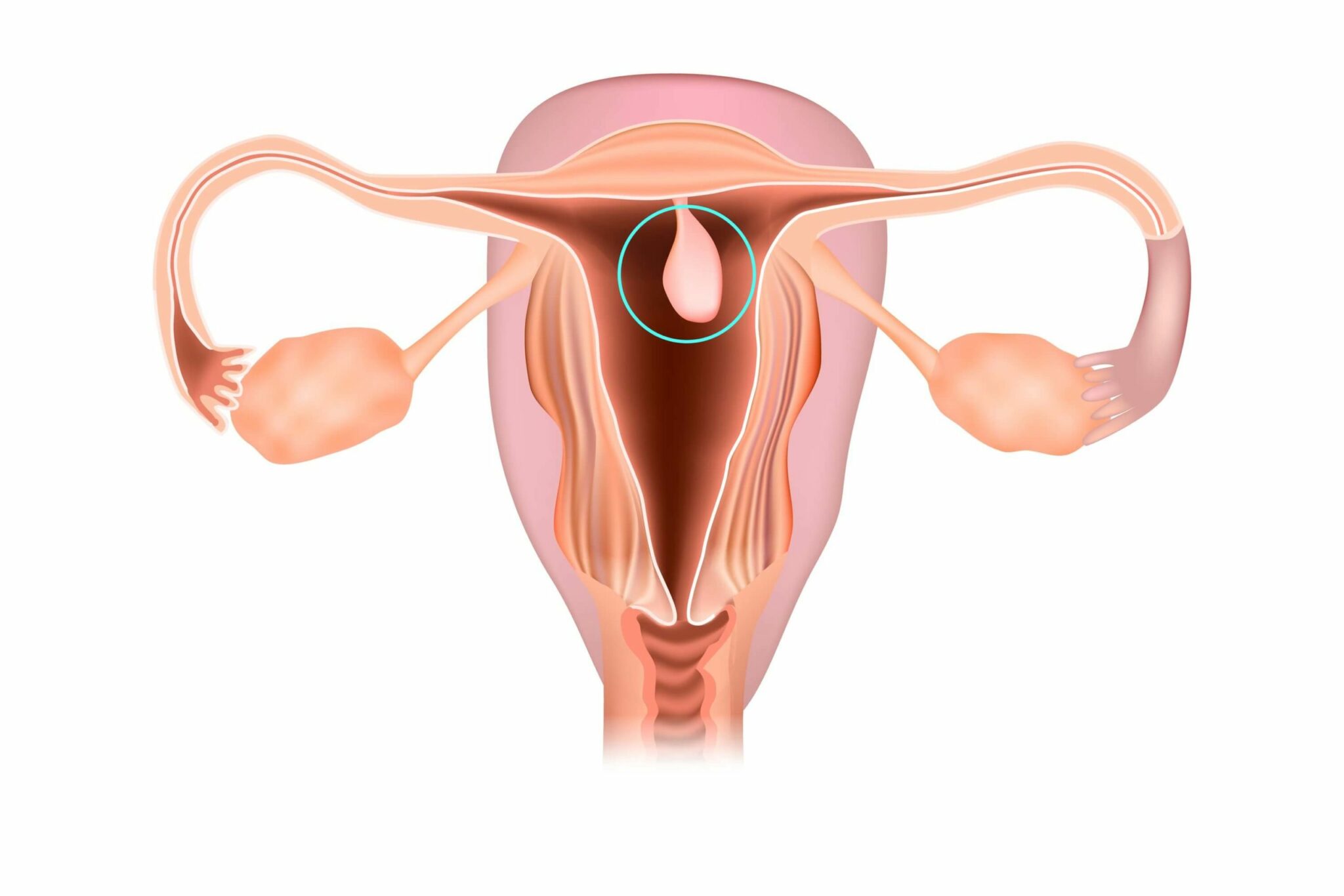
- Uterine polyps can arise in the neck of the uterus, the cervix (cervical polyps) or the lining of the uterine cavity (endometrial polyps).
- Relatively common, polyps are usually benign, often asymptomatic and don’t need to be removed.
- Two key symptoms of polyps are unusual bleeding (irregular periods, heavy periods, bleeding between periods) and infertility.
- Older women are more likely to develop polyps.
What are polyps?
Polyps are the most frequently observed structural abnormality of the female reproductive tract, affecting up to 10% of the female population. They can range in size from a few millimeters to filling the entire uterine cavity, and will either lie flat against the lining of the uterus (sessile polyps), or project from the endometrium via a stalk (pedunculated polyps). The growth rate of polyps can also be highly variable; some will grow steadily over time, others will actually regress.
Polyps are usually diagnosed using transvaginal ultrasound or hysteroscopy, with the latter technique considered to be the more accurate. An endometrial biopsy will usually be performed to assess whether the polyps are benign. With few clinical symptoms, polyps are often only uncovered following investigative procedures for unexplained infertility. In fact, the two main symptoms of polyps are:
- Abnormal uterine bleeding (irregular periods, heavy periods, spotting between periods)
- Infertility.
Polyps have been implicated in up to 50% of cases of abnormal bleeding and 35% of infertility cases. Premenopausal women are less likely to experience abnormal bleeding that is related to polyps than older women.
Risk factors and Causes of Uterine Polyps
It is not always known what causes polyps to develop.
- Age is a major factor and polyps are rarely found in women below 30. Recent work suggests that polyps might exist in a latent state in younger women, with those that do form being more prone to regression as the cells of the endometrium undergo continual cycling.
- Medication. Whilst the exact mechanisms that lead to the formation of uterine polyps is unclear, there is a strong association between their development and oestrogen. Women who are prescribed Tamoxifen or Hormone Replacement Therapy (HRT) are at increased risk of polyp formation. Tamoxifen is a partial oestrogen agonist used in the treatment of breast cancer. The incidence of endometrial polyps in women who have been prescribed tamoxifen is thought to be between 5 and 35%. HRT is frequently prescribed for menopausal women to alleviate some of the most uncomfortable symptoms. The oestrogenic effects exerted by tamoxifen on the uterus, and the continuous, unopposed stimulation of the endometrium that occurs with HRT, can both give rise to oestrogen-dependent polyps. Upon removal, these polyps have been found to contain increased numbers of oestrogen receptors.
- Obesity is an additional risk factor for polyp development because adipose tissue contains high levels of an enzyme called aromatase, which converts circulating androgens into oestrogens.
- Genetics. Not all polyps are hormonally-driven. Apoptosis, or the process of controlled cell death, has been proposed as one of the regulatory mechanisms responsible for ensuring the endometrium is shed with each menstrual cycle. There is evidence that apoptotic activity is reduced in polyp tissue, which could explain why these growths are not shed with the rest of the endometrial lining during menstruation. Furthermore, chromosomal abnormalities and differing genetic activity have been found in some women with polyps; particularly affected are those genes that regulate cell growth. Further work on the involvement of genes in polyp formation is required, to discern whether there is a familial, heritable component to the condition.
- Inflammation has also been proposed as a potential risk factor, with the suggestion that polyps occur as a result of localised tissue inflammation.
Polyp Removal
The gold standard treatment approach for those polyps that are causing physical discomfort or contributing to difficulties in conceiving is for patients to undergo a hysteroscopic polypectomy. This is a relatively simple technique that involves removal of the polyp tissue. Cervical polyps can often be removed using forceps; larger endometrial polyps may require cauterisation. Once removed, the recurrence rate is relatively low and complications are rare.
Dilation and curettage (D&C) is an alternative technique sometimes used for the treatment of uterine pathologies. It is not the preferred approach for polyps removal due to the high possibility of missing polyps during the procedure.
Women with polyps that are <10 mm in size are more likely to see natural regression over time and those who are asymptomatic may prefer to avoid surgical management altogether. However, in approximately 1% of cases, polyps can become cancerous, and therefore, women who opt not to have them removed, should undergo regular monitoring and screening to ensure that they remain benign.
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
Sources:
- Ben-Arie, Alon, et al. “The Malignant Potential of Endometrial Polyps.” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 115, no. 2, 10 Aug. 2004, pp. 206–210., doi:10.1016/j.ejogrb.2004.02.002.
- Chan, Ssc, et al. “A Randomised Controlled Trial of Prophylactic Levonorgestrel Intrauterine System in Tamoxifen-Treated Women.” BJOG: An International Journal of Obstetrics & Gynaecology, vol. 114, no. 12, Dec. 2007, pp. 1510–1515., doi:10.1111/j.1471-0528.2007.01545.x.
- Kanthi, Janu Mangala, et al. “Clinical Study of Endometrial Polyp and Role of Diagnostic Hysteroscopy and Blind Avulsion of Polyp.” Journal Of Clinical And Diagnostic Research, vol. 10, no. 6, June 2016, pp. QC01–4., doi:10.7860/jcdr/2016/18173.7983.
- Nijkang, Njume Peter, et al. “Endometrial Polyps: Pathogenesis, Sequelae and Treatment.” SAGE Open Medicine, vol. 7, 2 May 2019, doi:10.1177/2050312119848247.
- Wong, M., et al. “The Natural History of Endometrial Polyps.” Human Reproduction, vol. 32, no. 2, Feb. 2017, pp. 340–345., doi:10.1093/humrep/dew307.